What helps with varicose veins?
Author: Lucie Garabasova
Varicose veins affect the legs and lower limbs; they are twisted and enlarged veins. They are usually caused by genetic predisposition, but there are also factors that can trigger them. Although varicose veins are not life-threatening, they can cause uncomfortable symptoms. Fortunately, there are now many options available to alleviate the symptoms of varicose veins and improve the patient’s quality of life.
What are varicose veins?
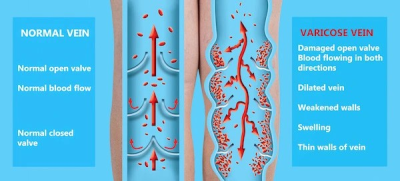
Varicose veins (varices) are a circulatory disorder affecting veins, primarily in the legs and lower limbs. Normally functioning veins ensure blood returns from the body to the heart. This process is supported by muscle contractions and valves within the veins, which allow blood to flow only toward the heart.
Varicose veins result from issues with blood circulation in the legs. In a healthy individual, veins transport blood from tissues back to the heart, working against gravity. They rely on a system of valves to prevent backflow, connections between deep and superficial vein systems, and the compression from surrounding muscles.
When this system fails, often due to weakened vein walls, blood pools in the vein, causing it to expand. In most cases, the accumulated blood and increased pressure on the vessel walls lead to enlargement and twisting of the veins, forming varicose veins.
In varicose veins, the affected veins are dilated, twisted, and function improperly. This condition can result from weakened vein walls and the inability of valves to effectively prevent backflow. As a result, blood remains in the veins, causing them to enlarge, discolor, and deform.
Symptoms of varicose veins
Varicose veins may cause unpleasant symptoms, such as:
- Visible, enlarged, and twisted veins: These are typically blue or purple veins visible beneath the skin’s surface and may bulge outward.
- Pain: Many people experience pain or discomfort in the affected area.
- Swelling in the legs and ankles.
- Fatigue and heaviness in the legs.
- Cramps and muscle tension.
Factors increasing the risk of varicose veins
Varicose veins can affect people of all ages and genders, but certain groups are more susceptible than others.
Women are most commonly affected, particularly during pregnancy and hormonal changes. Other at-risk groups include individuals with a family history of varicose veins, those in occupations requiring prolonged standing or sedentary work, and people who are overweight.
Varicose veins during pregnancy
During pregnancy, hormonal changes and the weight of a growing baby increase the likelihood of developing varicose veins.
This is due to:
- Higher levels of the hormone progesterone, which relaxes blood vessel walls and reduces valve function.
- A larger volume of blood in your body.
- Pressure from the baby on the pelvic veins, which can alter blood flow in the pelvic region and legs.
All these factors make it harder for blood to travel against gravity from your legs back to your heart.
In addition to varicose veins, constipation is also common during pregnancy and can lead to hemorrhoids.
How are varicose veins treated during pregnancy?
Since varicose veins are usually harmless and tend to improve after childbirth, healthcare providers typically do not treat them.
Instead, the focus is on alleviating symptoms and preventing further worsening.
You can help yourself by avoiding prolonged standing or sitting in one position, exercising regularly, reducing sodium intake in your diet, and occasionally elevating your legs to encourage blood flow back to your heart.
Did you know that sleeping on your left side can also help? This position reduces pressure on the inferior vena cava, a large vein that carries blood from your legs to your heart.
Do varicose veins disappear after pregnancy?
Yes, they are usually temporary and tend to shrink after the baby is born. However, if you have multiple pregnancies, they may worsen with each subsequent pregnancy or be less likely to disappear entirely.
If they persist after childbirth, be sure to contact your doctor to discuss suitable treatment options.
How can I prevent varicose veins?
You can prevent varicose veins through regular physical activity, maintaining a healthy weight, elevating your legs (especially if you have a sedentary job), following a balanced diet (consider incorporating hemp-based foods, such as hemp oil or seeds, which contain a balanced ratio of unsaturated fatty acids), and wearing proper footwear.
If you suspect varicose veins, visiting a doctor early can help initiate timely treatment.
What are the treatment options for varicose veins?
Treatment for varicose veins may include home care measures, compression stockings, surgery, or other procedures.
Procedures to treat varicose veins are often performed on an outpatient basis, meaning you can typically go home the same day.
Home care for varicose veins
Home remedies for varicose veins include exercising, elevating your legs while sitting, or wearing compression stockings. These measures can help alleviate pain and prevent the condition from worsening.
In addition to maintaining a healthy lifestyle, you can harness the power of herbs such as echinacea, milk thistle, gotu kola, or geranium. These herbs help cleanse blood vessels of deposits, which is essential for a healthy circulatory system.
Compression stockings
Wearing compression stockings all day is often the first solution to try and can be done independently at home. These stockings apply pressure to your legs, aiding veins and leg muscles in circulating blood more efficiently. The level of compression varies by type and brand.
Compression stockings are available at most pharmacies and medical supply stores. Prescription compression stockings, which may be covered by insurance if varicose veins cause significant issues, are also an option.
Ointment for varicose veins
You can also relieve varicose veins by applying suitable ointments or gels. These products help alleviate pain, swelling, cramps, and muscle tension.
Treatment of varicose veins
In addition to home remedies, it may sometimes be necessary to consult a doctor and begin treatment in a medical facility.
Surgery or other procedures
If self-care measures and compression stockings are ineffective or the varicose veins are more severe, your doctor may recommend surgery or other procedures:
Sclerotherapy
- This involves injecting a solution or foam into varicose veins, causing them to scar and close. Treated veins should fade within a few weeks.
-
Some veins may require multiple injections. Sclerotherapy doesn’t require anesthesia and can often be performed in a doctor's office as an outpatient procedure.
Laser Treatment
Laser treatment uses powerful bursts of light directed at the vein, causing it to fade and disappear over time. No cuts or needles are involved.
Of course, other methods are available, but these are the most common approaches.
How does CBD affect varicose veins?
CBD cannot cure varicose veins but can help alleviate the uncomfortable symptoms associated with them.
- Anti-inflammatory Effects: CBD has potential anti-inflammatory properties, which may help reduce inflammation linked to varicose veins and related symptoms.
- Muscle Relaxation: CBD may have relaxing effects on muscles and blood vessels, potentially improving blood flow in areas affected by varicose veins and alleviating feelings of heaviness and fatigue in the legs.
- Pain and Discomfort: CBD might help reduce pain associated with varicose veins and enhance overall well-being.
How to use CBD for varicose veins?
It is recommended to combine internal and external use of CBD for varicose veins.
- Internally: Apply CBD oil twice a day. Depending on the severity of the condition and your body weight, a 10% CBD oil or, for more significant issues, a 20% CBD oil is recommended.
In addition to internal use, it is beneficial to enhance the anti-inflammatory and harmonizing effects with an appropriate hemp-based topical product. We recommend using CBD Cooling Gel or CBD Coconut Oil.
How does Hemp Ointment work on varicose veins?
Hemp ointment is often used for relief from various types of pain and inflammation, although it is not specifically designed to treat varicose veins. It contains cannabinoids that interact with the body’s endocannabinoid system, potentially affecting pain perception and inflammation.
For varicose veins, the focus is typically on improving blood circulation, strengthening vein walls, and reducing inflammation. Hemp ointment could theoretically help alleviate pain, swelling, and inflammation associated with varicose veins, but it does not directly address weakened vein walls or the root cause of the condition.
Cannadorra recommends using their CBD ointment for varicose veins, which will soon be available in their product range!
How does Vitamin C affect varicose veins?
- Collagen Support: Vitamin C is essential for collagen production, a protein that forms the structure of blood vessels and connective tissue. Adequate Vitamin C intake can help maintain strong and elastic blood vessels.
- Antioxidant Properties: As a powerful antioxidant, Vitamin C can help reduce cell damage caused by oxidative stress. This may lower inflammation and support healthy blood flow.
- Vascular Health: Vitamin C promotes vascular health by enhancing blood vessel function and preventing blood clot formation.
What are the complications of untreated varicose veins?
Untreated varicose veins can lead to various complications, particularly in advanced or neglected cases. Below are some potential complications:
-
Venous Ulcers: Painful and difficult-to-heal sores that may develop near affected veins. These ulcers are prone to infection and often require long-term treatment.
-
Thrombophlebitis: Inflammation of the veins accompanied by the formation of a blood clot. This can cause pain, redness, and swelling near the affected vein. If the clot travels to deeper veins, it can lead to deep vein thrombosis (DVT), a serious condition.
-
Venous Wall Inflammation: Varicose veins can inflame the walls of veins, leading to pain, swelling, and skin thickening.
-
Hyperpigmentation: Excess pressure in the veins may cause skin discoloration, resulting in dark spots or patches.
-
Lipodermatosclerosis: This condition causes the skin around varicose veins to become hard, thickened, and discolored.
-
Cellulitis: Untreated varicose veins can worsen the appearance of the skin and contribute to the development of cellulitis.
-
Pain and Discomfort: Varicose veins left untreated can cause chronic pain, swelling, itching, and a heavy feeling in the legs, significantly impacting the quality of life.